Debunking UVGI Myths
INTERVIEW BY MARY KATE MCGOWAN, MANAGING EDITOR
 Ultraviolet germicidal irradiation (UVGI) can be used in conjunction with HVAC systems or in spaces to disinfect air and surfaces to reduce disease transmission, control biofouling of cooling coils in air handling units and improve indoor air quality (IAQ). The use of this technology escalated amid the COVID-19 pandemic, leading to increased questions and misconceptions.
Ultraviolet germicidal irradiation (UVGI) can be used in conjunction with HVAC systems or in spaces to disinfect air and surfaces to reduce disease transmission, control biofouling of cooling coils in air handling units and improve indoor air quality (IAQ). The use of this technology escalated amid the COVID-19 pandemic, leading to increased questions and misconceptions.
William P. Bahnfleth, Ph.D., P.E., Presidential Member/Fellow ASHRAE, and chair of the Epidemic Task Force, talked with ASHRAE Journal about the technology, misconceptions, best practices and resources. “Those who are selecting UVGI systems should first educate themselves about the fundamentals of the technology and understand how it is applied,” said Bahnfleth, who has taught ASHRAE Learning Institute’s “Introduction to Ultraviolet Germicidal Irradiation Systems” course and gives an ASHRAE Distinguished Lecturer presentation on UVGI fundamentals.
What are the most common misconceptions about UVGI?
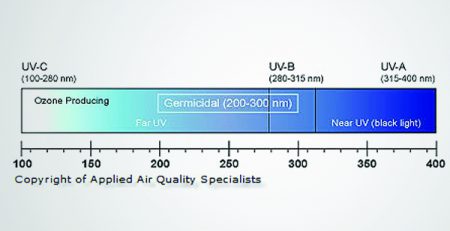
One common misconception is that germicidal lamps all produce ozone. It is true that the plasma in a mercury vapor or amalgam lamp produces a small amount of light at a wavelength of 185 nm that produces ozone, but this emission is easily filtered out by using the proper tube materials. Manufacturers have had no difficulty obtaining UL 2998 certification1 for their lamps. (UL 2998 validates that air cleaners emit zero ozone.) Only improper lamp selection will result in ozone production, and as LEDs that produce germicidal UV takeover from mercury vapor lamps (as it did in the case of lighting), there should be no risk of ozone production.
A second misconception is that germicidal ultraviolet disinfection is a new and unproven technology, including with respect to its ability to inactivate SARS-CoV-2, the virus that causes COVID-19 and other coronaviruses. The technology has been successfully applied to indoor air disinfection since at least the late 1930s,2 and it is approved for use in control of tuberculosis by the U.S. Centers for Disease Control and Prevention,3 which, through the National Institute of Occupational Safety and Health (NIOSH), has published guidelines for application of upper room systems.4
Are you seeing more people misapplying this technology when it comes to COVID-19 mitigation? If so, how are they misapplying the technology?
I would not say it is being misapplied, but perhaps some are not understanding the contribution to risk reduction it is making. Some air “purifiers” are marketed as including UVC. Many of these devices apparently use germicidal light to inactivate microorganisms captured on a HEPA filter. This could be viewed as beneficial by minimizing risk of re aerosolization of captured infectious particles, but probably does not materially add to the overall effectiveness of the device, since a HEPA filter removes nearly all entering particulate matter.
Germicidal UV installed in an air-handling unit is in series with whatever filters the system is required to have, so its incremental benefit will decrease as filter efficiency increases. For example, suppose a filter removes 60% of the viral load in an airstream on a single pass. If a UVGI airstream disinfection system is added that achieves 90% single pass inactivation, it is inactivating 90% of the infectious material that was not already captured by the filter. The removal efficiency of the combination is 96%, so the UVGI system only reduces the viral load by an additional 36% beyond what was captured by the filter. This does not make adding UVGI in such a situation a bad idea, but it needs to be understood.
What steps can people take to avoid misapplications?
Those who are selecting UVGI systems should first educate themselves about the fundamentals of the technology and understand how it is applied. The two ASHRAE Handbook chapters on UVGI5,6 are a good place to start. It is also very helpful to work with UVGI system manufacturers that have a record of successful installations.
What are your recommended best practices?
Most important, one must define the performance goals for a UVGI system, i.e., what dose needs to be delivered over what period of time for the design level of microbial susceptibility and under what ambient conditions—temperature and air speed. This defines the average fluence (the germicidal energy per unit area incident on a point in space from all directions) or irradiance (the germicidal energy per unit area at a point on a surface) that is needed and can be the basis for selecting an appropriate number and configuration of lamps. System design should be supported by calculations to confirm the required UV-C dose is delivered by the system. Manufacturers should be able to assist in this analysis.
What are some resources readers can use to learn more about best practices for using UVGI?
In addition to the ASHRAE Handbook chapters5,6 mentioned in response to Question 3, a 2008 ASHRAE Journal article summarizes best practices for mercury vapor lamp systems.7 The NIOSH guide4 for upper room systems mentioned in response to Question 1 is an excellent reference on that type of system. Kowalski’s book is a comprehensive source of information on many aspects of germicidal ultraviolet theory and application.8
Is there anything else you think engineers need to know about this topic?
The growing availability of germicidal LEDs that can produce different wavelengths within the UV-C band has the potential to greatly expand the ways in which germicidal light can be deployed in air and surface disinfection applications. Krypton-chlorine excimer lamps that produce 222 nm “far” UV-C are also an emerging technology of interest. Far UV-C light with a wavelength of approximately 220 nm and shorter is attracting a great deal of attention because preliminary studies suggest that it is not only an effective disinfectant, but also safe, or at least much safer for human exposure than the current 254 nm standard.9,10
References
- UL. 2019. “ECVP 2998, Environmental Claim Validation Procedure (ECVP) for Zero Ozone Emissions from Air Cleaners.” UL.
- Wells, W.F., M.W. Wells, T.S. Wilder. 1942. “The environmental control of epidemic contagion. I. an epidemiologic study of radiant disinfection of air in day schools.” American Journal of Hygiene, 35(1), pp.97 –121.
- Jensen, P.A., L.A. Lambert, M.F. Iademarco, R. Ridzon. 2005. “Guidelines for Preventing the Transmission of Mycobacterium Tuberculosis in Health-Care Settings, 2005.” “Morbidity and Mortality Weekly Report (MMWR).” Centers for Disease Control and Prevention.” https://tinyurl.com/y5jyqpjp
- NIOSH. 2009. “Environmental Control for Tuberculosis: Basic Upper-Room Ultraviolet Germicidal Irradiation Guidelines for Healthcare Settings.” DHHS (NIOSH) Publication Number 2009-105. National Institute for Occupational Safety and Health. https://tinyurl.com/y58n6oh5
- 2019 ASHRAE Handbook—HVAC Applications, Chap. 62, “Ultraviolet Air and Surface Treatment.”
- 2020 ASHRAE Handbook—HVAC Systems and Equipment, Chap. 17, “Ultraviolet Lamp Systems.”
- Martin, S.B., C. Dunn, J.D. Freihaut, W.P. Bahnfl eth, et al. 2008. “Ultraviolet germicidal irradiation: current best practices.” ASHRAE Journal 50(8):28 – 36.
- Kowalski, W. 2010. Ultraviolet Germicidal Irradiation Handbook: UVGI for Air and Surface Disinfection. Springer Science & Business Media.
- Welch, D., M. Buonanno, V. Grilj, I. Shuryak, et al. 2018. “Far- UVC light: A new tool to control the spread of airborne-mediated microbial diseases.” Scientific Reports 8(1):1 – 7.
- Woods, J.A., A. Evans, P.D. Forbes, P.J. Coates, et al. 2015. “The effect of 222-nm UVC phototesting on healthy volunteer skin: a pilot study.” Photodermatology, Photoimmunology & Photomedicine 31(3):159 – 166.
Source of Article: ASHRAE Journal (February 2021), Debunking UVGI Myths (https://www.nxtbook.com/nxtbooks/ashrae/ashraejournal_CKLLES/index.php#/p/Intro)